Challenges Facing Private Practitioners in 2024

The healthcare industry plays a vital role in society, meeting both routine healthcare needs and delivering life-saving emergency treatments. Driven by dedicated professionals, the industry takes pride in providing high-quality care to all. However, like any sector, it faces obstacles that can impede its ability to offer the best patient care.
In recent years, private practitioners in particular have been hit with numerous challenges, affecting not only their business operations but also their capacity to deliver exceptional care to patients.
What Is Private Practice?
A private practice is a healthcare business owned and operated by physicians or practitioners, rather than larger entities like hospitals or health systems. These practices are physician-run, and they vary in size—some are managed by a single doctor, while others operate as group practices, where multiple providers collaborate to run the business.
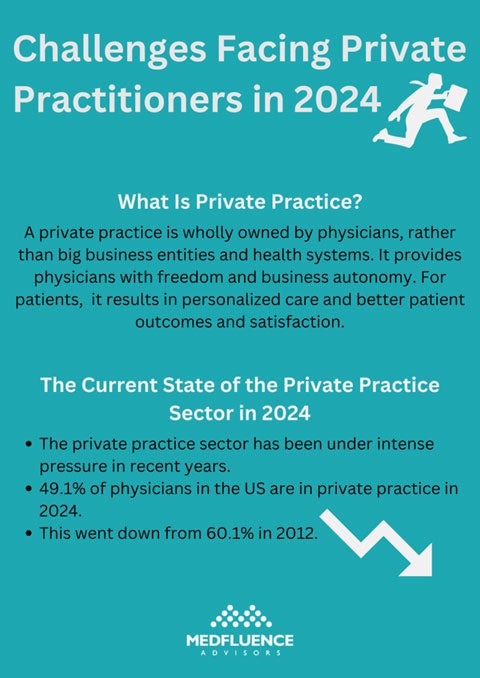
A private practice setting can be particularly fulfilling for practitioners due to the increased autonomy it offers. Unlike physicians in large hospitals or healthcare systems, who must adhere to strict institutional guidelines, those in private practices have greater freedom to make business decisions and shape their work environment according to their preferences.
More than that, private practices play an important role in the healthcare industry. For patients seeking medical care, private practices offer more personalized care. This results in better diagnosis and treatment, specifically tailored to each patient’s needs.
What Are the Advantages of Private Practice?
Going into private practice yields a lot of advantages such as:
Physicians Have Flexibility and Independence
One of the key benefits of private practice is the flexibility and independence it affords physicians. As owners of their practices, they have control over business decisions and the freedom to set their own work schedules. This level of autonomy is often constrained or non-existent in large hospitals and healthcare systems. The ability to manage their own schedules and make key decisions contributes to a healthier work-life balance for physicians in private practice.
Accessibility to Patients and Close Patient-Provider Relationships
Physicians in the private practice sector enjoy maximum accessibility to their patients, thus establishing a close patient-provider relationship. This allows them to provide continued care, resulting in better patient results.
When there is a close relationship between the patient and the provider, patients will feel more at ease and comfortable because they will feel that their physicians see them as people instead of just numbers and statistics moving through their business.
Superior Quality of Personalized Care
When practitioners establish a close relationship with their patients, this allows them to provide personalized care – and personalized care remains superior.
A major advantage of private practice is the flexibility and independence it provides physicians. As practice owners, they control business decisions and can set their own work schedules. This degree of autonomy is often limited or absent in large hospitals and healthcare systems. The freedom to manage their own time and make key decisions supports a better work-life balance for physicians in private practice.
Fosters Competition and Reduces Cost
In communities with multiple private practices alongside large hospitals, competition remains high, giving patients more choices for their medical care. This heightened competition benefits patients by keeping costs down, as they are more inclined to select facilities that meet their needs without straining their finances.
The Current State of the Private Practice Sector in 2024
The private practice sector is an important part of the healthcare industry. However, while it is crucial in maintaining this competitive landscape, private practitioners have been facing significant challenges in recent years. The pressures on private practices have intensified, compounding existing difficulties and impacting their ability to thrive.
The American Medical Association (AMA) released a recent Physician Practice Benchmark Survey. The survey showed that 49.1% of practicing physicians in the United States work and deliver patient care in private practices wholly owned by practitioners.
This number may seem good enough. However, the same AMA survey showed that this number went down from 2012’s 60.1% of physicians in the private practice sector. While private practices were already facing challenges, these issues were exacerbated by the onset of the COVID-19 pandemic.
When the pandemic took a turn for the worse, there was a sharp increase in physicians choosing employment with big hospitals, health systems, and other entities. This is due to the financial pressure the private practice sector faced at the height of the pandemic. Some physicians had no choice but to sell to acquiring entities and go into corporate practice instead. This factor – and more – have contributed to the decrease in the number of physician-owned private practices.
What Does This Mean for Patients?
The closing of several private practice facilities can lead to several issues concerning patients:
- It causes reduced access to care, especially in rural areas that rely on these private medical practices.
- The lack of close private practice facilities in rural areas will lead to increased travel distances for patients seeking medical care.
- Larger health entities and businesses often prioritize profit, so this can lead to poor patient outcomes.
What Are the Challenges Facing Private Practitioners in 2024?
Challenges in the private practice sector are not new. An AMA and Mathematica study enumerates and details these challenges. Here are some of the key challenges currently facing those in the private practice sector in 2024:

1. The Burden of Administrative Work
One major challenge many physicians face in the private practice sector is the burden of administrative work. Physicians in private practice have to balance between clinical responsibilities and administrative work.
There is a rise in the need for prior authorization, which is the payer’s requirement for a clinician to get approval for a certain procedure before providing it. It ensures that the insurance will cover the bill for the treatment.
Additionally, there are often administrative challenges in terms of coding and billing in private practices. The continuously changing administrative regulations can be overwhelming for a practicing physician who is balancing between clinical and administrative work.
2. The Problem With Getting Paid
The private practice sector is also suffering from low and declining payment rates from commercial insurers like Medicare and Medicaid. There is also a notable and drastic difference in how self-employed physicians in private practices are paid compared to those employed by larger health systems and hospitals.
Unfortunately, there is an ongoing trend that physicians in bigger healthcare systems and hospitals are paid much higher rates than private practice physicians, even if they deliver the same type of care to patients. This is due to their affiliation with major health systems, something private practice physicians do not have the luxury of.
3. The Rising Cost of Drugs and Medical Supplies
The cost of drugs and other medical supplies is rising, especially in recent years.
This poses a huge hurdle for private practices that are already operating on tight budgets due to varying factors. If this goes on, private practices will eventually have to raise patient prices to keep the business afloat.
4. Private Practices Often Lack Negotiating Leverage
Physicians in the private practice sector often face challenges in negotiating contracts with commercial insurers and feel there is a lack of negotiating leverage on their side.
Because the medical business is privately owned, there is often a lack of resources to renegotiate contracts to their advantage. It can also be difficult to make these insurer companies hear what they have to say in terms of contracts.
To solve this issue, many private practices hire additional personnel to do the contract negotiating for the business. But even this solution is costly and not many practices can afford to do so.
5. Recruiting Physicians and Medical Staff Is Challenging and Costly
All private practices must hire a few physicians, medical staff, and administrative staff but this can be challenging and costly for the business.
Starting the recruitment process to hire new personnel can take longer and cost more, making it difficult to fill open positions.
There are a few reasons why recruitment in private practice has been difficult:
- There is a lack of funds for recruitment advertising, physician salaries, and staff onboarding.
- Not all private practices are located in desirable business locations.
- Recruits are often more attracted to the higher salaries and enhanced benefits bigger health systems offer.
6. Difficulty in Collecting Data
The healthcare industry and the health systems inside it are responsible for collecting and analyzing population-based data and managing high-risk patients. Unfortunately, those in the private practice sector are having a more difficult time doing this.
Collecting and analyzing data can be time-consuming, and with the added demands of clinical and administrative duties, physicians in private practice often find they lack the time for this essential task. To manage data effectively, they may need to hire additional staff or invest in new resources, which can be costly, particularly for smaller practices.
7. It and Digital Costs
Today’s modern healthcare facilities and organizations are digital and use electronic health records (EHRs) in their systems. Purchasing digital systems and keeping them updated can be very costly, especially for small private practices. The lack of IT support after the purchase also presents a challenge for many physicians in the private practice sector.
There are a few big names in healthcare IT like Athena and Epic, but they often come with a hefty price so private practices are often forced to settle with low-cost IT solutions that don’t offer the same quality of service.
8. The Continuous Rise of Telemedicine
When the COVID-19 pandemic hit years ago, there was a sharp increase in telemedicine. This allowed patients to consult with medical professionals without having to meet face to face.
Even when the world went back to business as usual, telemedicine did not go away. Many patients still prefer the convenience of digital and online consultation, especially because they’re a cheaper way to go about one’s health. Telemedicine is here to stay and it is putting more pressure on the private practice sector who lose patients to it.
9. Professional Isolation Can Become a Problem, Too
Operating an independent practice can become professionally isolating. People have the desire to network with other people, especially those working in the same field. Professional connection and networking will allow medical practitioners to build communication and rely on each other for professional advice. Private practice can make this difficult, resulting in physicians feeling isolated from other practitioners and professionals in the medical field.
10. Mentoring Can Be an Issue
Mentoring is essential for recent graduates to help them smoothly transition to practice. This can be a challenge for solo practice physicians when there is a lack of fresh graduates to mentor. Being located in small or rural locations can also exacerbate this challenge, both for willing mentors and mentees.
What Is Being Done to Address These Challenges?
The American Hospital Association (AHA) has submitted a statement to the Committee on Ways and Means on the collapse of the private practice sector and the challenges that independent medicine is currently facing.
The statement includes laying out the burdens of increased costs, inadequate reimbursements, and administrative burdens and what they mean for physician-owned private practices. The AHA statement also explained how these challenges and their role in several private practices shutting down can affect patients.
AHA, in the same statement, recommends the following policies to address these healthcare challenges:
- Commercial Insurer Accountability: This policy aims to reduce administrative challenges like prior authorization to reduce administrative staff burnout and delay to providing care.
- Physician Payment Reform: This recommends legislative and regulatory changes to ensure a more sustainable payout and reimbursement.
- Provider Well-Being: This is to urge Congress to support the Dr. Lorna Breen Health Care Provider Protection Reauthorization Act (H.R. 7153/S. 3679), which addresses healthcare worker well-being. It provides grants to allow healthcare organizations to offer behavioral health services to prevent healthcare worker burnout and suicide.
Read more about the AHA statement in full here.
Conclusion: Private Practice and Its Challenges in 2024
The private practice sector is an integral part of the healthcare industry. Unfortunately, this area of the industry has faced a lot of challenges that hindered many physician-owned practices from being able to provide the quality patient care they had once provided.
Even with all the advantages of physician-owned medical practices, these recent challenges have forced many to cease operation and instead look for positions in bigger hospitals owned by business entities.
This has opened up a lot of issues in the healthcare industry and has undeniable negative effects on patients as well.
AHA has recognized this problem and has asked Congress to take action and address these challenges so that this integral part of the healthcare industry remains thriving to serve the community.